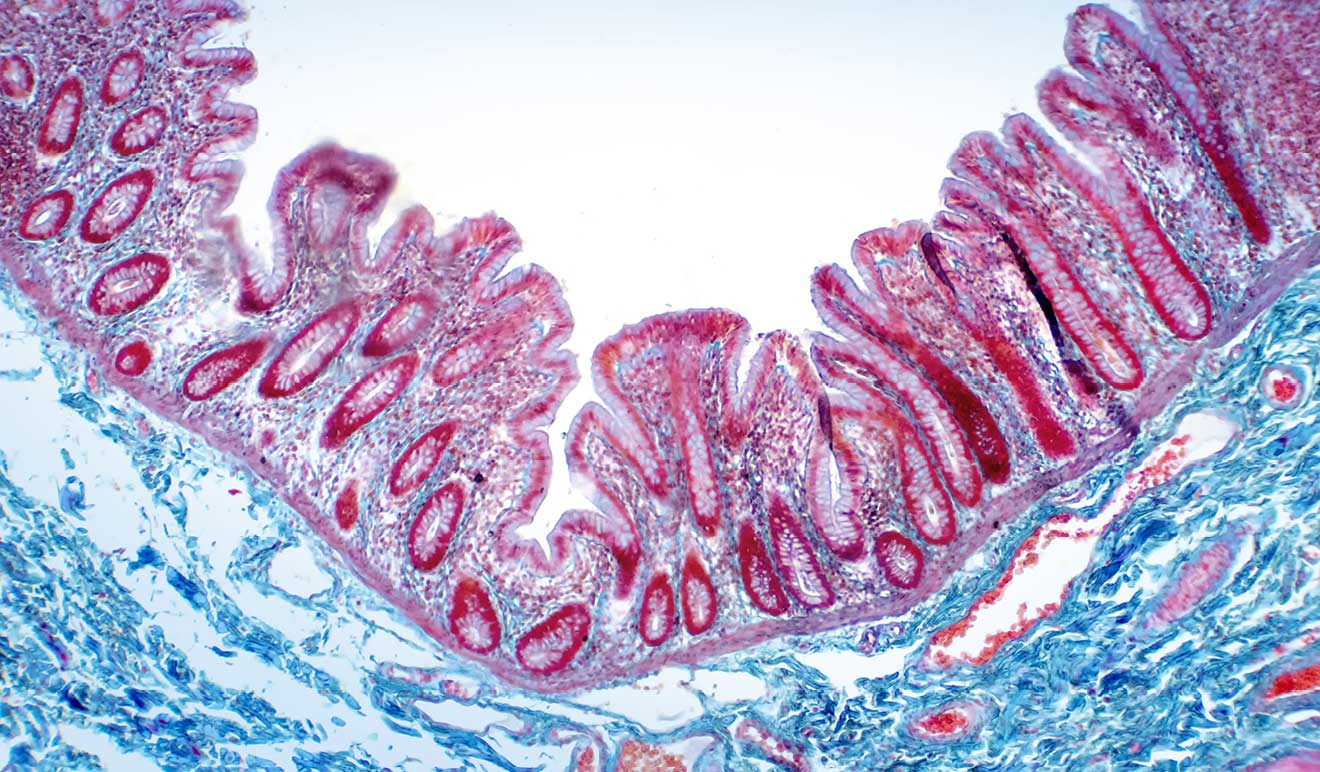
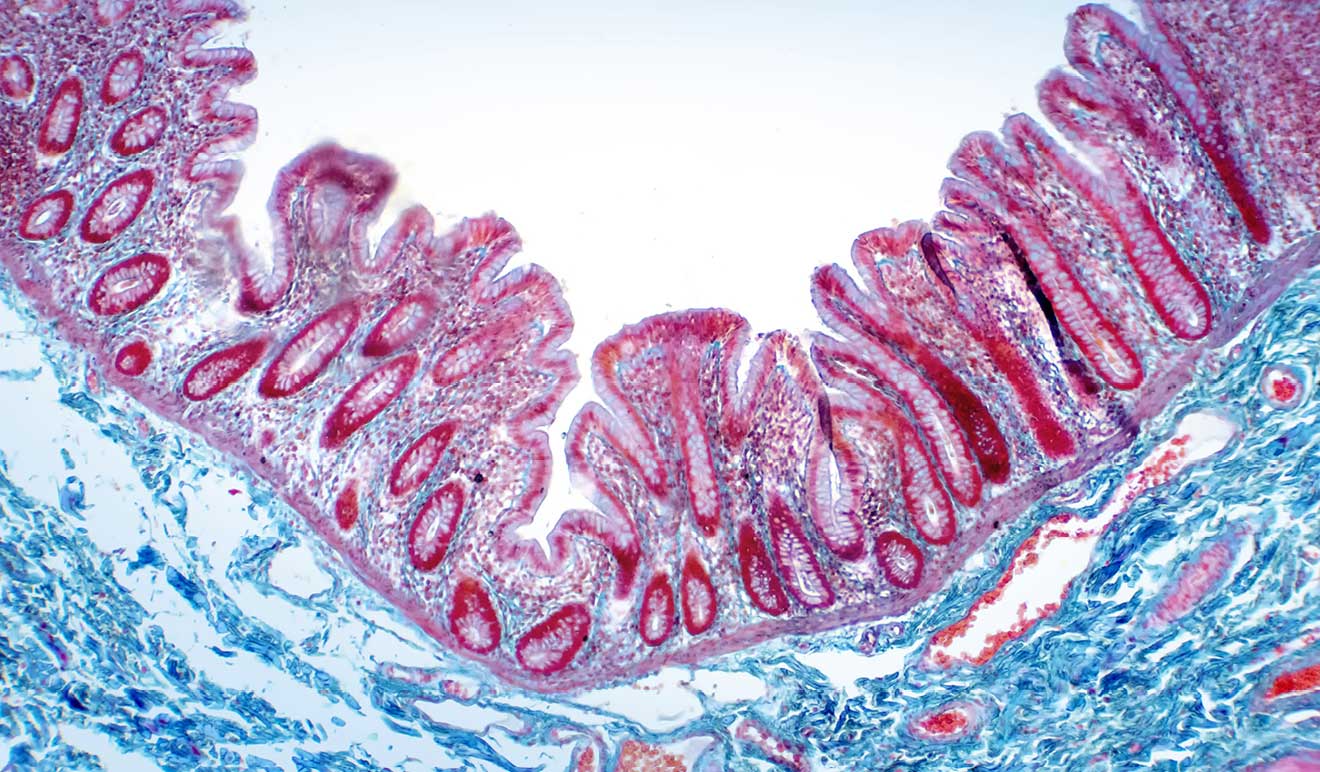
Increasing investigations into host-microbiota interactions have revealed that the intestinal microbiota is a critical mediator in maintaining health (Holmes et al., 2011).
Generally the “gut microbiota” is the diverse microbial community (bacteria, fungi, archaea, viruses and protozoa) that colonize the gastrointestinal tract of their host (Shukla et al., 2017).
The composition of the gut microbiome is similar at the phylum level (mainly Bacteroidetes and Firmicutes), but the diversity and species richness tends to vary between individuals (Tremaroli and Backhed, 2012).
Increasing investigations into host-microbiota interactions have revealed that the gut microbiota is a critical mediator in maintaining health (Holmes et al., 2011).
Generally the “gut microbiota” is the diverse microbial community (bacteria, fungi, archaea, viruses and protozoa) that colonize the gastrointestinal tract of their host (Shukla et al., 2017).
The composition of the gut microbiome is similar at the phylum level (mainly Bacteroidetes and Firmicutes), but the diversity and species richness tends to vary between individuals (Tremaroli and Backhed, 2012).
The factors that determine the structure of the microbiota are: host genetics, environmental factors, diet, stress, diseases (Shukla et al., 2017). While it is precisely the microbiota that determines the health and diseases of the host through genes, proteins or metabolites (Shukla et al., 2017).
Physiological energy homeostasis is regulated by the microbiota. For example, Donohoe et al. (2011) reported that butyrate produced by the microbiota provides energy to colonocytes and thus prevents autophagy in the colon. Furthermore, physiological homeostasis can be disrupted by the microbiota but this leads to: disruption of host metabolism, immune dysregulation, neurological and cognitive dysfunction and more (Roy and Trinchieri, 2017).
This altered state would cause a number of disorders, including obesity, diabetes, autoimmunity, allergy, inflammatory bowel disease (IBD), and cancer (Holmes et al., 2011; Buret, 2016). Emerging data on the gut microbiota reveal that it is involved in several diseases via the gut-brain axis (Baruch and Schwartz, 2016), the gut-lung axis (Budden et al., 2017; Shukla et al., 2017), the gut-liver axis (Nicolas et al., 2017; Xue et al., 2017), the gut-bone axis (Ohlssone Sjogren, 2015; Yan et al., 2016; Ridler, 2017; Villa et al., 2017), the intestinal-vascular axis (Zhu et al., 2016; Li et al., 2017) and other axes.
Microbiota-host communication in pathologies
Since the gut microbiota is in the gastrointestinal tract, it is evident that it too can contribute to intestinal pathologies (Holmes et al., 2011). However, emerging evidence shows that the microbiota is also implicated in extra-intestinal organs, based on different bacterial compositions. The alteration in composition could be attributed to diet or environment (cold, antibiotics, use of probiotics and onset of infections) and dominate the physiological state of the host.
More fundamentally, the communication pathways between the intestine and other organs are mediated by direct neuronal contact, enteroendocrine cells, immune cells and microbial metabolites (Schroeder and Backhed, 2016).
This role of the microbiota as a balance between health and disease is due to the different control functions it performs:

In practice, the microbiota operates as a control unit, and is also able to carry out physiological functions such as:

Regulation of blood pressure
(Yang T, Zubcevic J. Gut-Brain Azix in Regulation of Blood Pressure. Front Physiol. 2017 Oct 25;8:845).

Shapes cholesterol levels
(Gérard P. Metabolism of cholesterol and bile acids by the gut microbiota. Pathogens, 2013 Dec 30;3(1):14-24.)

Cardiac functions
(Luedde M, Winkler T, Heinsen FA, RÜhlemann MC, Spehlmann ME, Bajorovic A, Lieb W, Franke A,
Oct SJ Frey N. Heart failure is associated with depletion of coreintestinal microbiota.
ESC Heart Fail. 2017 Aug;4(3):282-290)

Kidney functions
(Jiang S, Xie S, Lv D, Wang P, He H, Zhang T, Zhou Y, Lin Q, Zhou H, Jiang J, Nie J, Hou F, Chen Y.
Alteration of the gut microbiota in Chinese population with chronic kidney disease.
Sci Rep. 2017 Jun 6;7(1):287)0)

Neuroendocrine system
(Farzi A, FrÖhlich EE, Holzer P. Gut
Microbiota and the Neuroendocrine System. Neurotherapeutics. 2018 Jan;15(1):5-22)

And it is no coincidence that the microbiota has been found altered in many,
if not all, the pathologies listed below.

Parkinson's
(Qian Y, Yang X, Xu S, Wa C, Song Y, Qin N, Chen SD, Xiao Q. Alteration of the fecal microbiota
in Chinese patients with Parkinson's disease. Brain Behav Immun. 2018 Mar 2, pii: S0889-1591(18)30028-X).

Alzheimer's
(Di Sabatino A, Lenti MV, Cammalleri L, Corazza GR, Pilotto A. Frailty and the gut. Dig Liver Dis. 2018 Mar 16)

ALS
(Brenner D, Hiergeist A, Adis C, Mayer B, Gessner A, Ludolph AC, Weishaupt JH
The fecal microbiome of ALS patients. Neurobiol Aging. 2018 Jan;61:132-137.)

MS
(Tremlett H, Waubant E. Gut microbiome and pediatric multiple sclerosis.
Mult Scler. 2018 Jan;24(1):64-68.)

Autism
(Campion D, Ponzo P, Alessandra C, Saracco GM, Balzola F.
Role of microbiota in the autism spectrum disorders. Minerva Gastroenterol Dietol. 2018 Mar 30.)

Metabolic Diseases
(Clavel T, Desmarchelier C, Haller D, Gérard P, Rohn S, Lepage P, Daniel H. Intestinal microbiota
in metabolic diseases; from bacterial community structure and functions to species of pathophysiological relevance.
Gut Microbes. 2014 Jul 1;5(4):544-519)

Indeed, Di Sabatino et al. report that different alterations of the microbiota,
which lead to different inflammatory responses,
lead to different pathologies such as Alzheimer's or Parkinson's.

Ultimately, beyond the present symptoms, it may be useful to strengthen the microbiota.